Spinal Stenosis
What is spinal stenosis?
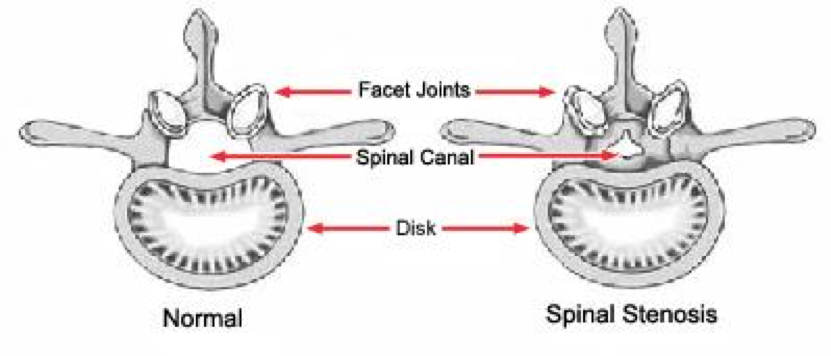
Spinal stenosis is a chronic condition that causes pain in the low back, buttocks, thighs and lower legs. It can significantly limit daily activities. The primary cause is osteoarthritis which causes degenerative changes in the structures around the spinal canal and the vertebral discs, facet joints and spinal ligaments.
Degenerative changes usually begin in the intervertebral discs which can herniate into the spinal canal causing pain and spinal instability. As degeneration continues, the discs compress and flatten shifting weight to the facet joints. The tunnels where the nerves exit from the spinal canal become smaller. The added pressure on the facet joints causes them to degenerate.
The damage stimulates the body to grow new bone (bone spurs) to stabilize the spine. But bone spurs grow into the spinal canal. These changes cause narrowing of the spinal canal which compresses the spinal cord and nerve roots. Further degeneration of the ligaments in the spine contribute to spinal stenosis and impinge on nerve roots creating the symptoms of pain, cramping, weakness and numbness. Compression of the spinal canal and nerve roots causes neurologic deficits. This is called Radiculopathy.
Who is at risk for spinal stenosis?
Spinal stenosis commonly occurs in adults over age 60. But degenerative changes of the spine are visible by x-ray in 95% of people by age 50. In younger people spinal stenosis is caused by trauma, scoliosis, and genetic diseases. If untreated, spinal stenosis can cause permanent damage.
Symptoms
Symptoms include pain, tingling, numbness, paresthesia, and weakness. Symptoms are typically related to activity and are initiated with prolonged standing and walking. Pain at rest is the result of longstanding untreated lumbar stenosis. In about 25% of people, lumbar spinal stenosis occurs simultaneously with cervical spinal stenosis. Aging muscles, heavy body weight and a sedentary lifestyle contribute spine instability and degeneration of the spine.
Diagnosis
Your Ortho Illinois orthopedic surgeon will conduct a complete physical exam, discuss your symptoms and order imaging tests like x-rays, MRI and CT scans.
Treatment
Nonsurgical treatment
Nonsurgical treatment is focused on restoring function and relieving pain. Over the counter pain medications, physical therapy, stability and mobility exercises, heat and cold treatments.
Epidural injections
Epidural injections of steroids may be used for diagnostic purposes, or for treatment of pain and inflammation.
Surgery
Surgery is designed to decompress the compressed nerves. When the symptoms get worse, surgery is the best option. It may involve removing a piece of bone or part of a herniated disc to relieve pressure and create more space for the spinal cord. New minimally invasive decompression techniques are available to reduce the damage to surrounding tissue which means recovery is faster and reduced hospital stays.
At Ortho Illinois we offer science-based protocols that emphasize the best non-surgical treatment options to restore function and avoid surgery. When surgery is unavoidable our fellowship trained spine specialists Drs. Braaksma, Stanley, Broderick and Alexander have the skills, training and experience to address herniated discs.
Ortho Illinois is a Regional Spine Care Center with offices in Rockford, Algonquin, and Elgin, Illinois. Call us and schedule consultation to get an accurate diagnosis and the least invasive, least aggressive options to relieve your pain.
